The process of attempting to achieve pregnancy, commonly referred to in medical and social circles by the acronym TTC or Trying to Conceive, represents a significant physiological and psychological phase for millions of couples worldwide. While the biological drive to reproduce is a fundamental human experience, the path to successful conception is governed by a complex interplay of hormonal timing, lifestyle variables, and age-related factors. Clinical data suggests that while the majority of couples will conceive within a standard timeframe, a significant minority requires medical intervention, highlighting the importance of preconception education and health optimization.
Statistical Overview of Conception Success Rates
According to data published by the American Society for Reproductive Medicine (ASRM) and the Centers for Disease Control and Prevention (CDC), approximately 85% of couples will achieve pregnancy within one year of regular, unprotected intercourse. This statistic serves as the baseline for clinical fertility. However, the remaining 15% of the population faces challenges that may necessitate the assistance of reproductive endocrinologists or fertility specialists.
Age remains the most critical non-modifiable factor in fertility. For women, fertility begins to decline gradually in their late 20s and more rapidly after the age of 35. By age 40, the probability of conception per menstrual cycle is estimated to be less than 5%. For men, while the decline is less abrupt, advanced paternal age is increasingly linked to decreased sperm quality and potential neurodevelopmental risks in offspring. Consequently, medical guidelines recommend that couples seek professional evaluation after 12 months of unsuccessful attempts if the female partner is under 35, or after six months if she is over 35.
The Biological Chronology of the Fertile Window
Successful conception is dependent on the precise synchronization of intercourse with the female ovulation cycle. The "fertile window" is biologically narrow, typically spanning a maximum of six days per month. This window includes the five days preceding ovulation and the day of ovulation itself.
The chronology of a typical 28-day menstrual cycle places ovulation around day 14, though clinical observations indicate significant variability. Ovulation may occur as early as day 10 or as late as day 22 in healthy individuals. Identifying this window requires a sophisticated understanding of biological markers:
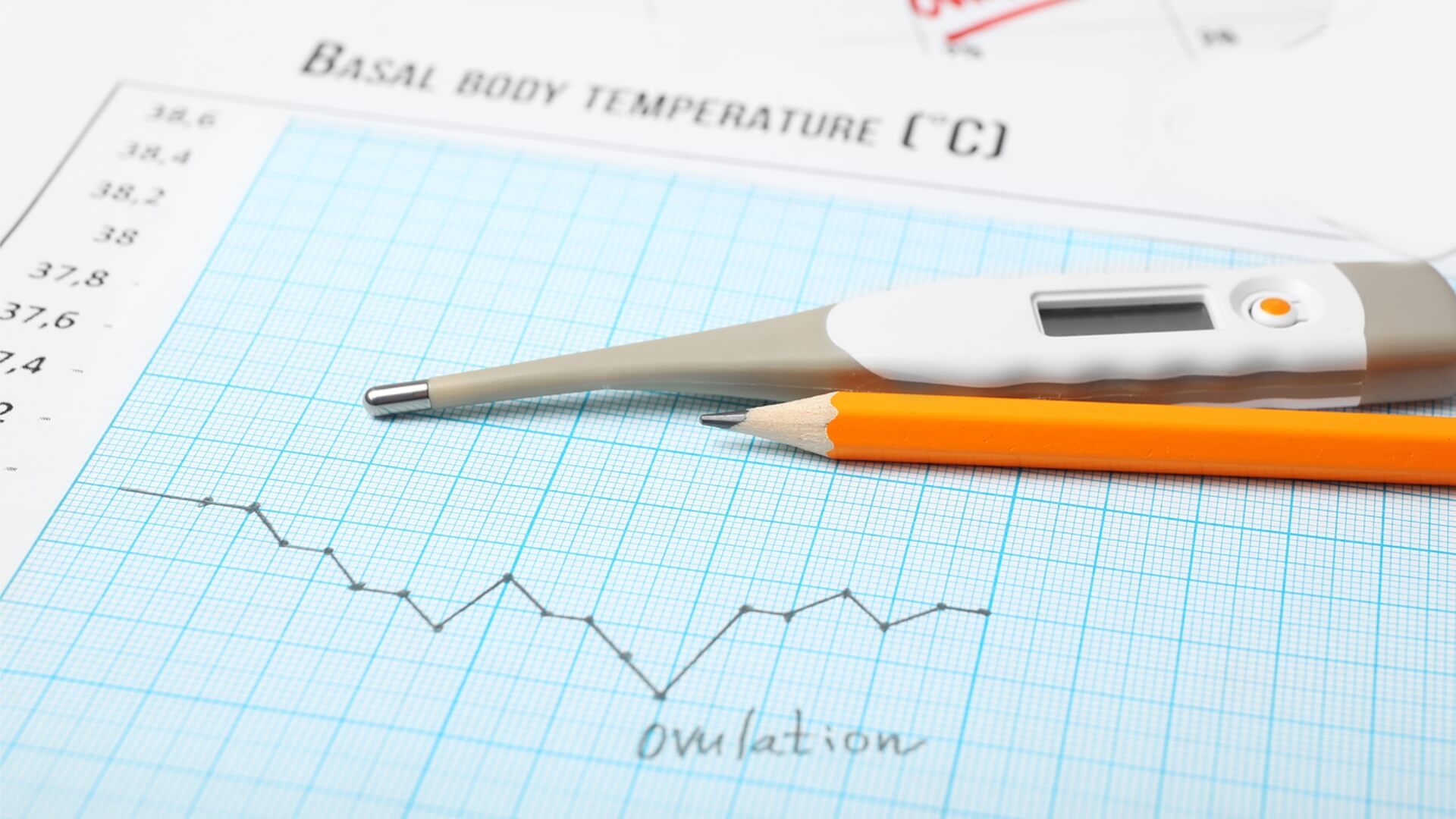
- Basal Body Temperature (BBT): A slight rise in resting body temperature occurs immediately after ovulation due to increased progesterone. While useful for tracking patterns, BBT is a retrospective indicator, meaning it confirms ovulation has already occurred.
- Cervical Mucus Changes: As estrogen levels rise leading up to ovulation, cervical mucus transitions to a clear, slippery, "egg-white" consistency. This physiological change facilitates sperm transport and survival.
- Luteinizing Hormone (LH) Surge: Ovulation prediction kits (OPKs) detect the surge in LH that occurs 24 to 48 hours before the egg is released, providing a proactive signal for timed intercourse.
Sperm cells can survive within the female reproductive tract for up to five days under optimal conditions, whereas the ovum (egg) remains viable for only 12 to 24 hours post-release. Therefore, clinical recommendations emphasize having intercourse in the days leading up to ovulation to ensure sperm are present in the fallopian tubes when the egg arrives.
Clinical Recommendations for Coital Frequency and Technique
To maximize the probability of fertilization, the American Pregnancy Association and other leading health organizations suggest a frequency of intercourse every other day during the fertile window. This cadence ensures a consistent supply of healthy sperm while avoiding the physical and emotional exhaustion that can accompany daily attempts.
While popular culture often emphasizes specific positions for conception, medical literature indicates that there is no definitive "best" position. However, remaining supine for approximately 15 minutes following intercourse may theoretically assist sperm retention near the cervix. Furthermore, the choice of lubricants is a critical but often overlooked factor. Traditional water-based lubricants often have a low pH and high osmolality that can inhibit sperm motility. Couples are advised to utilize "fertility-friendly" lubricants that mimic the pH and consistency of cervical mucus.
Gender-Specific Health Protocols for Preconception
The health of both partners contributes equally to the likelihood of a healthy pregnancy. Preconception care is now recognized as a vital component of maternal and infant health outcomes.
Maternal Health Requirements
For women, the primary focus is on stabilizing the endocrine system and ensuring nutrient density. The supplementation of folic acid (at least 400 mcg daily) is mandatory to prevent neural tube defects, which occur in the earliest weeks of gestation, often before a pregnancy is confirmed. Additionally, maintaining a Body Mass Index (BMI) within the "normal" range (18.5 to 24.9) is associated with more regular ovulation. Both underweight and overweight statuses can trigger hormonal imbalances that disrupt the hypothalamic-pituitary-ovarian axis.
Paternal Health Requirements
Male fertility is often neglected in the TTC narrative, yet "male factor" infertility contributes to approximately one-third of all cases. Sperm production, or spermatogenesis, takes roughly 64 to 90 days. Therefore, lifestyle changes made by the male partner today will not manifest in sperm quality for nearly three months. Men are advised to avoid excessive heat (such as hot tubs or tight-fitting clothing), which can impair sperm count, and to incorporate antioxidants like Zinc, Selenium, and Vitamin C to protect sperm DNA from oxidative stress.
Environmental and Lifestyle Modifiers
Modern research has identified several environmental factors that act as endocrine disruptors, potentially lowering fertility in both genders. Phthalates and Bisphenol A (BPA), commonly found in plastics and certain personal care products, have been linked to reduced egg quality and lower sperm counts.
Dietary habits also play a foundational role. A "Mediterranean-style" diet—rich in monounsaturated fats, whole grains, legumes, and fish—has been clinically shown to improve fertility outcomes. Conversely, high intakes of trans fats, processed sugars, and excessive caffeine (more than 200mg per day) are associated with increased time to conception. Substance use, including tobacco and alcohol, is strictly discouraged; tobacco use, in particular, is known to accelerate the depletion of a woman’s ovarian reserve and damage sperm morphology.
The Psychological Impact and Support Systems
The TTC journey is frequently characterized by high levels of psychological distress. Studies have compared the stress levels of women struggling with infertility to those of patients diagnosed with cancer or chronic hypertension. The repetitive cycle of hope and disappointment can strain interpersonal relationships and lead to "intercourse on demand" stress, which may ironically decrease the frequency of intimacy.
Health professionals advocate for a holistic approach that includes stress management techniques such as mindfulness, cognitive-behavioral therapy (CBT), or support groups. Maintaining open communication between partners is essential to ensure that the process of trying to conceive does not overshadow the foundational relationship.
Broader Implications and the Role of Medical Intervention
The global shift toward delayed parenthood has increased the demand for Assisted Reproductive Technology (ART). While lifestyle modifications and timing are effective for many, they cannot overcome structural issues such as blocked fallopian tubes, severe endometriosis, or azoospermia (absence of sperm).
The analysis of current reproductive trends suggests a growing need for early fertility screening. Proactive testing of Anti-Müllerian Hormone (AMH) levels for women and semen analysis for men can provide couples with a realistic roadmap, allowing them to bypass months of unsuccessful natural attempts if underlying issues are present.
In conclusion, the journey of trying to conceive is a multifaceted endeavor that requires biological literacy and lifestyle discipline. By optimizing health, understanding the nuances of the fertile window, and recognizing when to transition from natural attempts to clinical assistance, couples can significantly improve their chances of achieving a successful pregnancy. As reproductive science continues to evolve, the emphasis remains on early education and the mitigation of modifiable risk factors to support the transition into parenthood.