The landscape of maternal healthcare is undergoing a significant transformation as expectant parents increasingly prioritize autonomy and informed consent through the use of structured birth plans. Historically viewed by some medical staff as a source of friction, the birth plan is being reimagined through visual templates designed to bridge the communication gap between patients and clinical teams. As obstetric practices evolve to emphasize patient-centered care, the adoption of concise, icon-based "visual birth plans" has emerged as a critical tool for improving the labor and delivery experience. These documents serve as a blueprint for the preferences of the birthing person and their partner, ensuring that the healthcare team can support the family’s choices regarding medical interventions, environment, and neonatal care without disrupting the physiological process of labor.
The concept of a birth plan—a written document outlining a parent’s preferences for labor, delivery, and postpartum care—first gained prominence in the 1980s as a response to the highly medicalized nature of hospital births. In the decades prior, birthing individuals often had little say in the interventions performed during delivery. The rise of the natural birth movement encouraged women to take an active role in their care. However, traditional birth plans often consisted of several pages of dense text, which medical professionals found difficult to navigate during the fast-paced and often unpredictable environment of a hospital labor ward. This disconnect frequently led to birth plans being overlooked or dismissed by staff, sometimes resulting in a breakdown of trust between the patient and the provider.
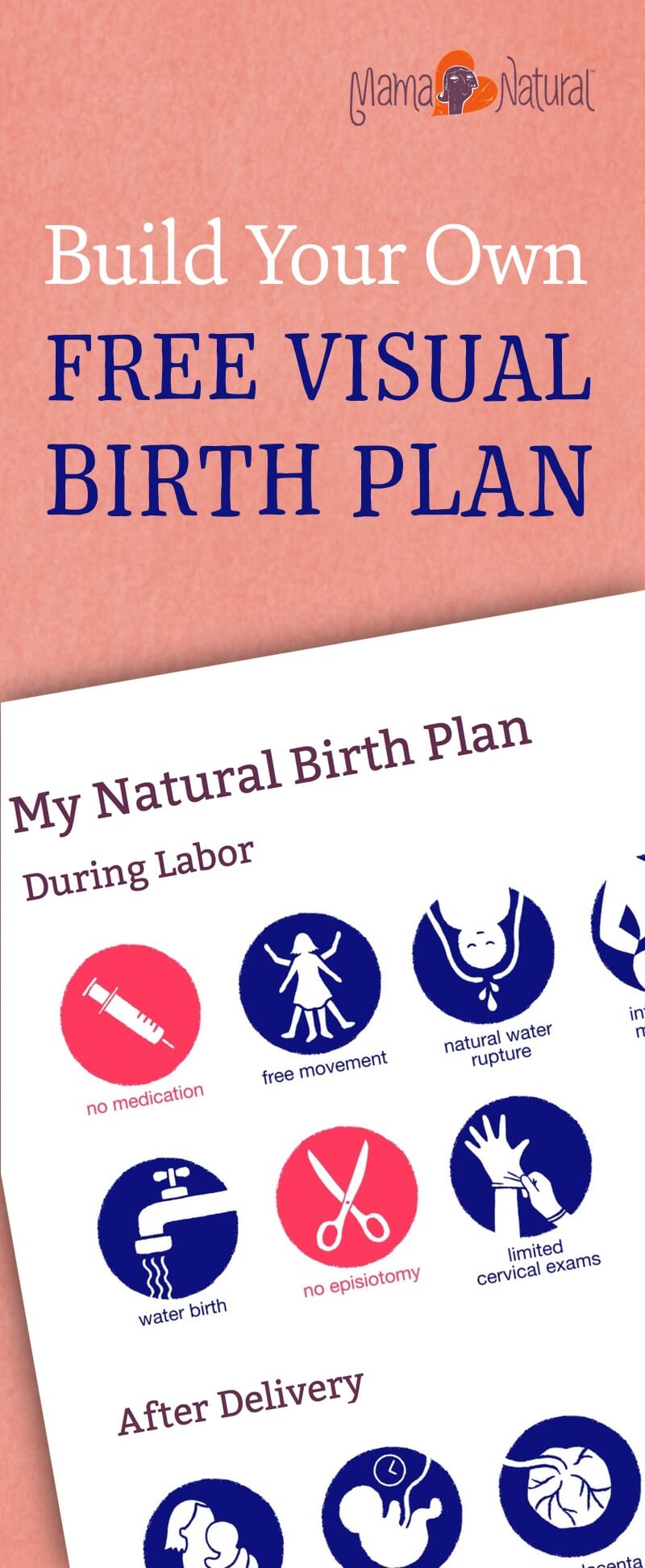
To address these challenges, the modern "visual birth plan" has been developed as a streamlined, one-page alternative. These templates utilize a system of standardized icons to represent various preferences, such as freedom of movement, intermittent fetal monitoring, and delayed cord clamping. By condensing complex desires into a series of easily recognizable graphics, these templates allow nurses, midwives, and obstetricians to understand a patient’s primary goals at a glance. This shift toward visual communication is supported by cognitive load theory, which suggests that in high-stress environments, such as a delivery room, medical staff are more likely to process and retain information presented visually rather than through lengthy narrative text.
The implementation of these tools comes at a time when maternal health outcomes are under intense scrutiny in the United States and globally. According to data from the Centers for Disease Control and Prevention (CDC), maternal mortality rates remain a significant concern, with stark disparities affecting women of color. Advocacy groups, such as the National Association to Advance Black Birth (NAABB), have highlighted the importance of tools like the Black Birthing Bill of Rights to empower patients and ensure respectful, high-quality care. Within this context, a birth plan is not merely a list of preferences but a safeguard for patient rights and a mechanism for reducing unnecessary medical interventions that can lead to complications.
The visual birth plan template, such as the widely utilized version provided by Mama Natural, categorizes preferences using a color-coded system to further enhance clarity. Blue icons generally represent "positive" preferences—actions the birthing team is encouraged to take, such as allowing the use of a birthing ball or practicing immediate skin-to-skin contact. Conversely, red icons signify "negative" preferences or interventions the patient wishes to avoid unless medically necessary, such as an episiotomy, the routine use of Pitocin, or the immediate bathing of the newborn. This binary visual system allows for rapid assessment by the clinical team, ensuring that the "black and white" preferences of the family are respected even as shifts change or new personnel enter the birthing suite.
The evolution of these templates in 2025 includes specialized icons for "Gentle Cesareans," reflecting a broader medical trend toward making surgical births more family-centered. A gentle cesarean may include preferences for a clear drape (allowing the mother to see the birth), the playing of specific music, and the immediate placement of the infant on the mother’s chest while the surgical procedure is completed. By including these options in a standard birth plan, patients can prepare for various outcomes, ensuring their voices are heard even if the birth deviates from their original "natural" goal.

Despite the benefits, the reception of birth plans among medical staff remains a subject of debate within the obstetric community. Qualitative studies and anecdotal evidence suggest that some nursing staff perceive detailed birth plans as a sign of an "inflexible" or "high-maintenance" patient. This stigma often stems from the unpredictable nature of childbirth; medical providers may fear that a rigid plan will prevent necessary life-saving interventions. However, proponents of visual plans argue that a well-constructed, simple document actually facilitates better medical care by establishing a baseline of mutual respect. When a patient presents a concise, one-page visual guide, it signals to the medical team that the patient is informed and prepared, while also acknowledging the need for the document to be "readable" under pressure.
From a clinical perspective, the most effective birth plans are those discussed with the primary healthcare provider—whether a midwife or an obstetrician—well in advance of the due date. This prenatal consultation allows for a "meeting of the minds," where the provider can explain hospital policies and the patient can express their non-negotiables. For instance, if a hospital’s standard of care includes continuous fetal monitoring, a patient desiring intermittent monitoring can negotiate this during a prenatal visit, using the visual plan as a reference. This proactive approach reduces the likelihood of "surprises" during active labor, a time when the birthing person is least able to advocate for themselves effectively.
The broader implications of visual birth plans extend to the psychological well-being of the parents. Research in the field of maternal psychology indicates that a sense of "perceived control" during labor is a primary factor in preventing birth trauma and postpartum depression. When parents feel that their choices were respected and that they were active participants in the decision-making process, they report higher levels of satisfaction with the birth experience, regardless of whether medical interventions were ultimately required. In this sense, the birth plan serves as a psychological tool that fosters a sense of agency in a situation that is inherently beyond one’s total control.
Furthermore, the rise of the "birth doula" as a standard member of the birthing team has reinforced the utility of visual plans. Doulas often act as the primary advocates for the birth plan, using the document to remind hospital staff of the patient’s wishes during the intensity of labor. A visual template is particularly useful for doulas and partners, as it provides a quick reference guide that can be posted on the wall of the labor room, ensuring that every staff member who enters the room is immediately aware of the family’s priorities.
As the healthcare industry continues to move toward digitized records, the integration of birth plans into Electronic Health Records (EHR) is the next logical step. Some hospitals have already begun allowing patients to upload their visual birth plans directly into their patient portals, ensuring that the document is accessible to any provider within the hospital system. This digital integration helps to standardize the use of birth plans and reduces the risk of the physical document being lost during a hospital transfer or an emergency.
In conclusion, the transition from long-form, narrative birth plans to streamlined, visual templates represents a significant advancement in obstetric communication. By prioritizing clarity, brevity, and mutual respect, these tools address the historical tensions between patients and medical providers. While no birth plan can account for every possible scenario in the unpredictable journey of childbirth, the visual birth plan provides a robust framework for shared decision-making. As medical systems worldwide strive to improve maternal outcomes and patient satisfaction, the visual birth plan stands as a testament to the power of simple, effective communication in the pursuit of a safe and empowered birthing experience. The continued refinement of these tools, including the addition of icons for diverse birthing scenarios and the emphasis on health equity, ensures that the birth plan will remain a cornerstone of modern maternity care for years to come.